Mid-sized to large medical practices seeking an all-in-one EHR and billing solution with enterprise-level RCM capabilities. Starts at $110/provider/month for core billing, with full practice management bundles from $300-$500+/month based on practice size; custom enterprise quotes available. Free cloud-based EHR with integrated medical billing, e-prescribing, and scheduling for small to medium-sized practices. This comparison table simplifies decision-making by detailing key features, pricing structures, and usability to guide readers toward the right https://www.bookstime.com/ tool. Mid-to-large medical laboratories handling high test volumes and needing integrated LIS with full revenue cycle management. Practice management and EHR system offering lab billing, insurance verification, and revenue cycle tools.
- Our expert medical billing services can take the stress out of your practice.
- The ICD-10-CM code set is updated annually by the CDC’s National Center for Health Statistics (NCHS), usually with an October 1 effective date.
- Large hospital labs or integrated health systems needing enterprise-scale billing integrated with EHR.
- Remittance Advice (RA) is a crucial document in the healthcare revenue cycle management (RCM) process.
- Treat the RA not just as a payment record but as a source of insight, and it will help boost revenue capture, cut denials, and build better working relationships with payers.
- The explanation for the reason code will be in the Glossary section of the Remittance Advice.
Are you a member looking for a provider?
The medical billing revenue cycle is quite complex and, if not managed correctly, could have negative financial implications for healthcare organizations. Due to its complexity, many healthcare providers significantly experience challenges optimizing the medical billing processes when scaling the business. Remittance advice sits at the center of healthcare revenue cycle work.
- However, it may take longer if there are any questions or issues with the documentation submitted.
- This may be due to existing workflows or a lack of digital infrastructure.
- With a user-friendly interface and industry experts available for all your billing, payments, and collections needs, BillFlash is the perfect solution for small practices.
- Medical billing codes change constantly, and codes are frequently deleted or added.
- The software emphasizes compliance, accuracy, and cash flow optimization through automated workflows and real-time reporting.
Difference between Remittance Advice (RA) and Explanation of Benefits (EOB)

Effective Jan. 1, 2026, MCOs must reimburse health care providers for gross receipts taxes they pay on Medicaid services. West Plan Codes ReportFind more information about the UnitedHealthcare West Plan Codes Report and NICE system. Automated Clearing House (ACH)/direct deposit Learn more about this option, also known as electronic funds transfer (EFT), in our enrollment guide. It outlines why it’s preferred by most practices because of its speed and efficiency in depositing payments directly into a bank account. Each payment is issued for the full amount of the claim payment at no charge to you. Our digital solutions are designed to give you the most up-to-date claims status and payment information quickly and easily.
- This field will display an amount of $0 on duplicate provider remittance advices even when the original showed a payment amount.
- While providers focus on patient care, another pressure point intensifies behind the scenes — seasonal healthcare billing surges within medical and…
- When viewing the total for the GRP/RC-AMT column, note that any amounts that have a group code of CR, or are listed as a previously paid amount, will be excluded from this total.
- This section identifies what portion of the balance can be billed to the patient, such as deductibles or coinsurance.
- Solo practitioners or small clinics seeking a cost-free EHR with basic billing tools integrated into clinical workflows.
- It makes sure that providers are being paid and by billing patients accurately and correctly.
Claims Adjustment Reason Codes (CARCs) and Remittance Advice Remark Codes (RARCs)
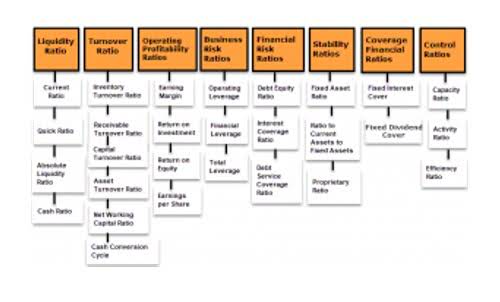
CARCs provide the basic reasons why an insurance company adjusts a payment. For example, a claim may be denied due https://fsafresno.com/2023/04/06/solved-identify-the-variable-costs-fixed-costs-and/ to incorrect information or if a service is not covered under the patient’s insurance plan. CARCs make corrective actions on payment discrepancies much easier for medical practices. They help providers identify why a claim was not paid in full and what steps need to be taken to resolve the issue.

ERAs are typically received through remittance advice a claims clearinghouse that integrates with practice management systems (PMS) or EHR. This integration provides a detailed breakdown of payments, helping healthcare providers identify discrepancies or issues during payment reconciliation. Adopting ERA streamlines payment processes and enhances financial management for healthcare providers.
- Effective use of remittance advice improves revenue cycle management and ensures timely, accurate payments.
- It supports ANSI 5010 formats, HIPAA compliance, and integrates with numerous EHR and practice management systems.
- Differentiating between RA and EOB is important to avoid confusion, as they serve distinct purposes and have different recipients.
- Understanding these codes is essential for navigating the remittance process effectively.
- With advanced analytics and AI-powered insights, Kareo helps providers achieve higher clean claim rates, often exceeding 98%, while supporting specialties like behavioral health and therapy.
Understanding these codes is essential for navigating the remittance process effectively. Verifying that payments match the services rendered helps maintain the financial health of healthcare organizations through remittance advice. These codes, including CARCs and RARCs, further explain the transaction summary.